
Special observations and methods of assessment of a patient who has dyspnea include: auscultation of the chest for abnormal breath and voice sounds, lung aeration, rales, and rhonchi inspection of the chest for respiratory rate and rhythm and for symmetrical expansion inspection of the skin, lips, and nail beds for cyanosis and percussion of the chest for abnormal resonance.
#Living with paroxysmal nocturnal dyspnea how to
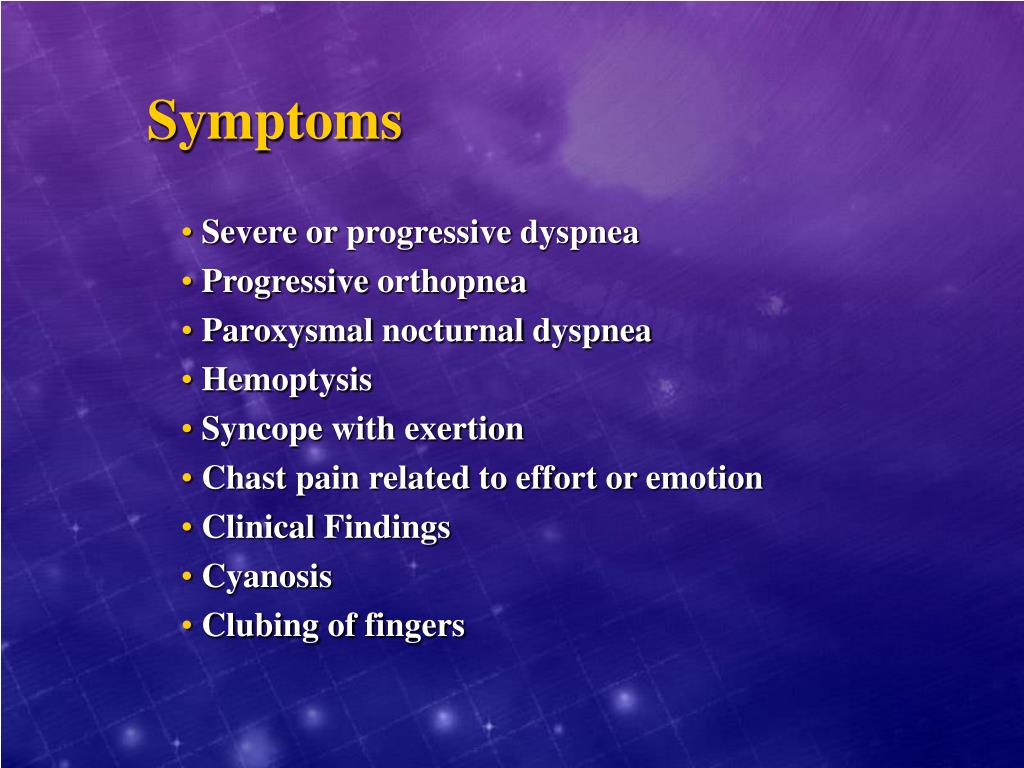
If they already know how to do pursed-lip breathing (inhaling slowly through the nose and exhaling slowly through pursed lips), they may need to be reminded of it and encouraged to use it to improve breathing. Once dyspneic patients are comfortable and less apprehensive, they may need instruction in prolonged, controlled exhalation. Orthopnea, paroxysmal nocturnal dyspnea, edema: Congestive heart failure, chronic obstructive pulmonary disease: Medications: Beta blockers may exacerbate bronchospasm or limit exercise tolerance. The medical term for this symptom is paroxysmal nocturnal. If abdominal distention, ascites, or a massive tumor interferes with chest expansion and produces dyspnea, having the patient lie on one side and supporting the abdomen with pillows may provide some relief. Some people with heart failure wake up in the middle of the night with severe shortness of breath. Helping the patient relax muscles not needed for breathing conserves oxygen and promotes rest. High Fowler's position or orthopneic position with the arms resting on pillows on an overbed table will help improve chest expansion. The patient should respond favorably to a calm, reassuring manner and an explanation of what is being done to relieve the shortness of breath. If the patient is suffering from an acute attack of dyspnea and has a history of chronic airflow limitation, certain nursing measures can help relieve anxiety and improve ventilation.
If there is airway obstruction, clearing the airway is necessary, or a tracheotomy may be performed. This usually occurs after several hours a person has fallen asleep and improves when they sit upright. This difficulty with breathing can cause a person to wake up gasping for air. In cases of acute respiratory distress, it may be necessary to intubate the patient, begin oxygen therapy, and obtain laboratory arterial blood gas data. Paroxysmal nocturnal dyspnoea is a condition that elicits sudden shortness of breath during sleep. If the patient is acutely short of breath, corrective measures should be instituted promptly. A current and past history are obtained and a physical examination completed as soon as possible. Whatever the cause of dyspnea, the plan of care begins with treating the patient and providing adequate oxygenation.Ī thorough assessment of the patient's condition is necessary in order to ascertain the extent of the problem and the urgency of the need.
The dyspneic patient has some degree of difficulty in meeting the basic physiologic need for adequate levels of oxygen in the blood and the transportation of that oxygen to all cells of the body.


 0 kommentar(er)
0 kommentar(er)
